
TAKE CHARGE OF YOUR MENTAL HEALTH RECOVERY
USE OF FLASH DRIVE FORMS
-Be A Solution-
It is recommended that the reader print the “Flash Drive Forms” and “Terms and Definitions” page prior to reviewing this online educational platform to aid one’s comprehension and understanding.

Section 1: Survey A (Recovery Holistic Care Considerations)
Preamble: With your treating physician, the recovery survey data loaded on these “Flash Drive Forms” is discussed to determine what “Recovery Holistic Care Considerations” can be implicated or ruled out.
Outcome: With the data collected from the Flash Drive Forms, an individual’s “Recovery Code Prescription” can be determined. See prescription form.
Overview
The holistic pillar of recovery orientation asks your treating physician to consider other recovery care constituents, as listed in Survey “A”, which research has demonstrated is attached to empowering mental health recovery through strengthening brain health.
The casting of Recovery Care Considerations captures a greater array of recovery factors connected to mental illness, outside of medications. In this survey, these considerations highlight hard and soft science disciplines that researchers have shown complement and cultivate not just recovery but can also enhance treatment outcomes. This approach brings science to the art of psychiatry.
The lens through which Citizen Psychiatry views its holistic approach to recovery is known as “Personal Medicine” or sometimes referred to as Precision Medicine. With “Personal Medicine”, the premise proposed is contained in the following.
In Personal Medicine, though the symptom classification of major psychiatric diagnosis is the same across the population base, the route contributing to these conditions for each person can look different from one individual to another. This means each person’s recovery needs to be individualized and personalized as opposed to the current practice of applying one treatment standard, neuro-chemistry medications, to fit everyone across the populous without taking into account each person’s unique blueprint. Add to this, psychiatry’s singular focus on the neurotransmitter model of major psychiatric illnesses as the sole means to explain and treat major mental illness with psychoactive medications, as if chemistry can account for the complexity of brain health gone awry, resulting in mental illness. “The Recovery Protocol Breakthrough” personalizes with greater precision the holistic parameters that support making a recovery achievable.
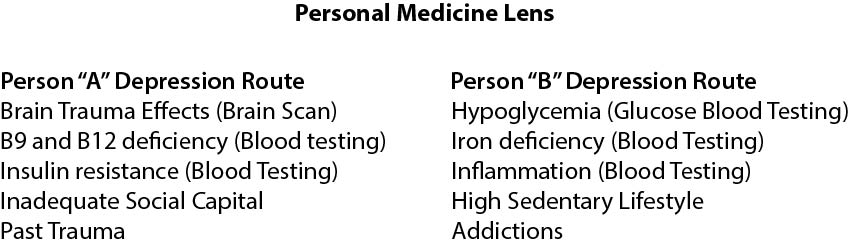
Consider in this example, depression. The symptoms are universal across the population but the routes to depression are manyfold. Under our “Recovery Care Considerations” (Flash Drive Forms, Section 1, Survey A), each person’s individualized blueprint for depression is going to look different from one person to another. Through investigating these care considerations, the results could show”.
The prescribed use of Zoloft or Paxil medications used to treat serotonin-based depression, for example, cannot treat the non-chemistry routes to this mental health condition directly. As a result, there is a large possibility that “treatment resistance” is the natural outcome.
As such, a holistic approach, outlined in “Recovery Care Considerations” spans beyond the chemistry of the brain as the sole factor in present-day street psychiatry’s approach to treatment as it neglects to take into account other significant recovery care factors connected to sustaining the life of major mental illness. This is how the occurrence of “treatment resistance” can occur with higher probability. Can citizens continue to afford to hold out for the right “Pill” to appear to kick start and sustain a recovery?
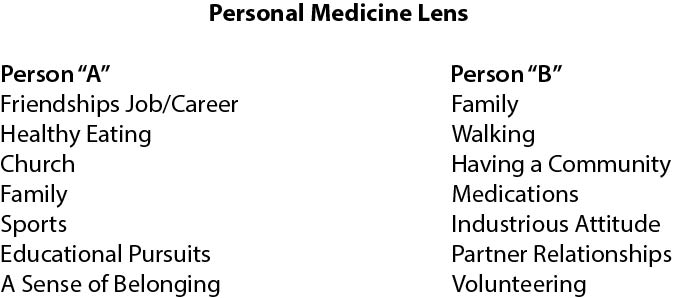
In another example, recovery drive factors (Section 1, Survey B) and hurdles to recovery (Section 2, Survey F, G, and H) offer the means to lay out an individualized plan highlighting key psychosocial variables of significance, contributing to sustaining the grip of the psychiatric condition while outlining generative forces linked to the recovery drivers that feed the person’s life. Consider regenerative practices to build brain health, which in turn, builds mental health. For Persons A and B from the previous example, this can look like:
Let’s take a brief tour of these holistic care considerations of the Holistic Recovery Care Consideration Bar (Section 1, Survey A).
a) Infectious Disease History: Numerous studies have linked a variety of infections in a person’s past as being associated with the emergence of various major mental health illnesses. This is one of the most underestimated data points to rule in or rule out. A person’s recovery and treatment approach would look differently if a previous infection is tied to their current illness.
b) Hope-Building Actions: “Hope” is critical to both treatment and recovery. Currently, the “Pill” is considered the only source of “hope” for the consumer to hang their hat on for psychiatric treatment. A twist on the proverbial saying, “don’t put all your eggs (Pills) in one basket” echoes what consumers ought not to do, but is the norm in psychiatry. As a result, this protocol widens the scope of hope-building actions as opposed to the sole reliance on the “pill” to pin one’s hope on. “Hope” is a recovery mindset requiring tending, like watering house plants.
c) Trauma History: It has been well-researched and documented for decades how histories of trauma can significantly contribute to forming and sustaining persistent major mental health illnesses. A thorough examination of past traumas is warranted, not just childhood abuse, but also traumas stemming from racism, stigma, poverty, war, religion, violence, accidents and other impactful events.
d) Brain Scans (Structural and Functional): These scans or mappings are hard science tools for modern mainstream psychiatry. On the research side of the psychiatric equation, grade A studies on functional imaging, like fMRI and SPECT, have shown how various brain areas and systems seen can elucidate the neuro-activity pattern connected to each person’s mental disorder experienced through a “Personal Medicine” lens. In neural mapping, hot and cool areas of brain functioning are illuminated to show a person’s own unique pattern of neural activity between various brain systems, some of which can have overlapping patterns across the population for major mental illnesses. This information is considered in conjunction with other relevant psychiatric and recovery factors. Structural scans, like CT, can be used to detect brain injuries, lesions, tumors, bleeding and infections, for example, that can be connected to psychiatric symptoms.
Though the use of brain scans or mapping with qEEG is still hotly debated for clinical use, various pioneering work has shown promise over the past few decades. In Canada for example, SPECT was approved in 2021 as a valid assessment tool for major psychiatric conditions by the Association of Nuclear Medicine, a bold step forward. And in Ontario, Canada, the state Medicare program covers the fees for SPECT.
Nutrition | Eating habits
While medication’s purpose is to affect the neurochemistry of the brain, the role of nutrients found in foods and eating patterns researched to date has gained greater prominence in demonstrating its contribution towards building back brain health associated with recovery from major psychiatric conditions.
For example, from a brain chemistry point of view, psychiatry drugs cannot manufacture neuro-messengers like serotonin or dopamine which are claimed to be at low levels causing depression. However, only proteins in foods can manufacture neurotransmitters. Serotonin drugs, like Zoloft, primarily trick the brain’s chemistry into thinking there is an adequate supply for sufficient functioning. In another example, fats are responsible for building the protective layer of nerve transmission cells which act like cables that allow the neuro-signals to travel from one nerve cell to another, critical for our ability to think, feel and move. The wrong fats consumed, like trans-fats, coming from fried foods over time, are incorporated in these cell’s membranes resulting in the disruption of neuro-transmission, and keeping the mental illness going strong.
No medications on the market can address these contributing factors by taking a “Pill”. Without addressing such routes, nutritionally linked “Pill” taking increases the probability of “treatment resistance”. (See Appendix for Resources)
Sedentary | Movement Ratio
It is well-researched and known how movement impacts the brain’s mental health status in treatment and personal recovery. The use of exercise is one form of movement along with walking and yoga, for example. What is not well taken into account is the role of sedentary behaviors. The effect of sitting and lounging for hours a day, day in and day out, whether at work or at home, can take away any health gains from sustained movement, like exercise. A look at the ratio of sedentary living versus movement living provides valuable data with which to provide direction toward empowering a person’s mental health recovery.
Head Impact History
Looking for possible brain injury from impact is one of the most missed and glossed-over of treatment and recovery data points. A review of a person’s history to determine whether there have been any past impact incidents to merit ruling in and or out further investigation is underrated in mainstream psychiatry unless there is an obvious brain trauma of note. This vital information, if missed, will have a profound impact on both treatment and recovery progress. One prevalent myth to keep in mind is that one needs to lose consciousness to have brain trauma or injury, but this is not true.
If no clear, obvious brain impact is recalled, that does not necessarily mean one or multiple impacts of significance did not occur. Collateral information can be sought by speaking with caregivers or siblings, of significance, for example. Here, childhood head injuries or impacts may have occurred but remain unrecognized. A diligent probing with questions is required.
Nature Quotient
Within the last 10 years, a huge push to research the effects of nature immersion, whether walking tree-lined parks or streets, hiking trails, listening to bird songs, or caring for household plants, has flourished. The results are in and for recovery and treatment purposes the higher one’s nature quotient, the more robust a person’s psychiatric and personal recovery. This may not be surprising, as we are more sedentary in our lifestyles than a mere 100 years ago and stay indoors more than outdoors, as well. This domain can no longer be overlooked.
Social Capital
Loneliness can exacerbate symptoms of a major mental health condition. It is one of the most overlooked factors in the “Treatment Room”. Taking medications cannot address loneliness. However, having safe intimate ties, whether with families, marriage, friendships, work, or through community involvement and peer support, can counter the weight of loneliness. The key to social capital is the ability to receive instrumental and emotional support which has weight, value and meaning that the individual can accept or conversely give to others.
It takes just one connection of significance, meaning and value that is active in an individual’s life to confer great benefits whether in person or virtual. This connection can be with professional support, like a psychotherapist and physician provider. As well, there is relational capital that can confer benefits such as one’s relational ties with pets, gardening, nature to activities of value like reading, knitting, puzzles, walking, music to sports and recreation, for example.
Blood Testing
Preamble: Blood testing is a hard science tool offering relevant wellness data impacting the brain’s mental health from a “Personal Medicine” lens perspective. This line of testing is the least understood and acted upon in mainstream psychiatry through decades of grade “A” research have shown how nutrient factors and the role of hormones, steroids, vitamins, fats, glucose, inflammation and minerals have been linked to major mental health illnesses and are key to both treatment and recovery as well. Why?
The gravitation towards psychoactive drugs, combined with the neurotransmitter theory of mental illness, was a technological breakthrough over 70 years ago. The novelty of this technological solution overshadowed parallel work in nutrition; for example, showing its contribution to both treatment and recovery. The formalization of psychiatry around drug technology has crowded out other peer-reviewed research looking at other contributors in the treatment and recovery equation, like nutrition. This means physicians and psychiatrists are only educated on drug use, focus on neurotransmitters, and neglect the importance of nutrient routes implicated in sustaining the mental condition.
Blood Testing (These are the same tests applied in psychical medicine but are interpreted for mental health illness.
a) Steroid hormones: cortisol, DHEA, estrogens (women), testosterone (men and women).
b) Non-steroid hormones: thyroid hormones (TSH, T3, T4).
c) Vitamins: B1, B2, B3, B5, B6, B 9, B12, Vit D, Vit C.
d) Fats (lipids): LDL/ HDL, omega -3 (EPA/DHA).
e) Minerals: copper, zinc, magnesium, ferrite, iron.
f) Inflammation (non-specific): highly sensitive C-Reactive Protein, Homocysteine; Glucose (tests).
g) Blood glucose: fasting insulin, fasting glucose, A1C, glucose tolerance test.
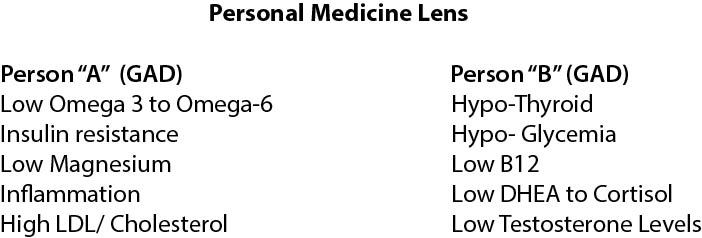
Using a Personal Medicine lens look at these two profiles below who are diagnosed with a GAD (Generalized Anxiety) mental disorder. As one can see, Person A pathways to GAD looks different from Person B’s but leads to supporting the symptom classification of GAD. (See appendix for Resources)
Sleep Quality
There is no mystery as to the impact of persistent poor sleep on a person living with mental health illness. The pain and suffering can be magnified with poor sleep quality whether due to insomnia, sleep apnea, restless legs, chronic pain, or by other disturbances. An inadequate sleep pattern has been noted across all major health illnesses and places a significant drag on recovery and treatment. This is one recovery domain that requires addressing by a sleep examination at first. It is important to eliminate any biological route to determine how to proceed. However, typically, this factor is often neglected in the treatment room but is a critical variable in making a recovery.
Section 1: Survey B
The purpose of collecting this recovery data is manyfold.
a) To provide the materials to apply “The Recovery Protocol”, program streams.
b) To review the current state of your mental health power holding your recovery alive.
c) To offer data on what recovery drivers can be strengthened, downgraded, eliminated and added.
d) To provide information to evaluate recovery progress.
e) To provide a menu for selecting the significant drivers of one’s recovery (Section 1, Survey C)
f) To quantify a scaling measure for what is called “The Uplifting Force”. This scaling offers a
way to look at the degree of “Lift” generated by the recovery drivers outlined.
g) To paint a landscape picture of recovery drivers and factors currently in play.
Survey C
In this survey, participants are asked to identify six recovery drivers that are most salient to their recovery from Survey “B” data. These identified “six” drivers become prime drivers that are then massaged further for their personal agency value. These drivers listed can be updated and changed over time.
Survey D
Here, you are introduced to quantifying a value known as the “Uplifting Force” associated with the impact of the recovery drivers on the whole, identified in Survey “B” and not just the Top 6 acknowledged. Such information is very useful for evaluating recovery progression and offers insight and awareness as to the strength of one’s mental health recovery power.
Section 2, Survey E
In this survey, you are identifying the “Hurdles” that are preventing an individual from making recovery progress. The data collected can be used to track factors of resistance, i.e., what hurdles are in, what hurdles are out, and what hurdle impacts need dampening. This survey paints a landscape of barriers. As well, this landscape provides a scaling measure for what is called “The Dragging Effect”, outlined below. This resistance produced by the hurdle’s “dragging effect” is quantified by scaling, to outline the weight load of the hurdles identified and carried as a burden of The Illness.
Survey F
This survey asks persons to state their six current barriers of significance, presently. These hurdles are selected from the general survey “E” identified. Frequent updates of these hurdles in play occur often as they are removed and other more relevant barriers can be placed on the list. As such, the list represents the current focus of attention.
Survey G
Here, you are introduced to quantifying a value known as the “Dragging Effect” associated with the impact of the hurdle’s weight in producing resistance to recovery. Such information is very useful for evaluating recovery progression and offers insight and awareness as to the strength of the hurdle’s impact on the “Uplifting Force” value ascribed in Survey D, Section 1, and how to counter the resistance from a recovery driver and Uplifting Force perspective.
Section 3
Survey H- Exercise 1
With this exercise, persons are asked to become more aware of what the significant recovery drivers, listed on their top six, offer in richness to their lives. While the treatment culture predominately values “what is wrong”, in this exercise, what is “working right” for a person is elevated and given merit in a more focused way. Acknowledging this richness can increase the worth and value of these drivers on the top six list. As well, as new drivers are placed on this list, their capacity for enriching constituents can be examined.
Exercise 2
This exercise’s data allows individuals to acknowledge and express to themselves, their personal care circle (family, friends, partner) and their treatment team what living with a mental health condition is like and that is not easily understood. The aim is to offer those of importance, further understanding and appreciation for what is being endured. The other aim is to assist in being understood and lessen the feeling of being alone. These two factors are key to supporting recovery endeavors. Also, for evaluative purposes, this information is useful by noting movement and progress.
Exercise 3
Similar to Exercise 2, this data allows an individual to express to their care circle and treatment team how their psyche is affected by living with a mental illness, day in and day out. The aim is to offer further understanding of the impact faced due to their mental health conditions. Also, for evaluative purposes, this information is useful to note progress.
Section 4: The Recovery Report Card
For the first time, consumers can evaluate and chart their recovery status and progression with this report card. Both the person and treating physician are asked to sign off on the report card. People can hold their treatment team to account. In addition, as a tracking tool, the report card would offer a marker for when changes are required, overall, in the Recovery Protocol Breakthrough in conjunction with other measures taken and suggest both what is working well and what is not.
“We are all in this together.”
-The Recovery Specialist
